Procedures

Dr. Kathleen Hands – Thyroid and Endocrine Center of South Texas
- Diagnostic US
- US Guided FNA
- LN Classification
- Cytopath
- Radioactive Iodine
- Thyrogen
- Thyroid Lab
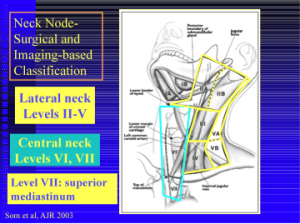
Neck Lymp Nodes Classification by Levels II-VII:
Current ATA guidelines state that low risk, stage I and II, Papillary thyroid cancer patients do not require radioiodine in most circumstances. This aggressive treatment is reserved for high risk patients in conjunction with Nuclear Medicine specialist.
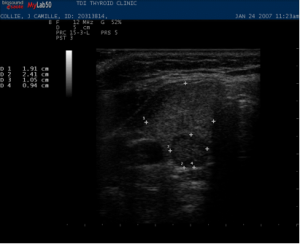
Malignant Thyroid Nodule:
D Cytopathology:
At the center, Dr. Kathleen Hands uses the ultrasound equipment to diagnose cancer by guiding the needle into selected areas of the suspicious nodule. This is called Fine Needle Aspiration Biopsy (FNA). As a thyroid cytopathologist, member of the American Society of Cytopathology, she prepares and evaluates the biopsy slides for adequacy to avoid unnecessary repeat procedures, reviews specimens with thyroid specific cytopathologists for expert review, requests immunostaining when appropriate and offers genetic testing when indicated.
Malignant Lymph node:
E. Radioactive Iodine (I-131)
I – 131 has been used for decades to treat hyperthyroidism and thyroid cancer. This is usually a one time treatment where you swallow a small capsule containing radioactive iodine. Since the thyroid is the only body part that uses iodine, I 131 is a targeted therapy to thyroid tissue alone. Dr. Hands oversees all I 131 treatments to ensure appropriate dosing and American Thyroid Association (ATA) guidelines are followed for the treatment of Graves and thyroid cancer.
F. Thyrogen (recombinant human TSH) is an injection medication (buttocks) used to prepare thyroid cancer patients for I-131 ablation. It is administered on the two days prior to receiving I-131. By giving you TSH “stimulation” the remaining cancer cells after surgery are primed to receive I 131. Prior to the advent of Thyrogen, this was traditionally done by removing your thyroid hormone suppression (stopping levothyroxine or Synthroid) for weeks before treatment to make you significantly hypothyroid. With use of thyrogen, you may remain on your thyroid medication, live a normal life without the long standing ill effects of being hypothyroid for your treatment period.
Although not FDA approved for goiters, Thyrogen is used to facilitate the treatment of large nodular goiters with I-131, in place of surgery. This can reduce the size of the goiter without surgery in patients where surgery may be risky.
G. Thyroid Lab
CLIA certified to process blood samples for TSH, free T4 (Thyroxine), free T3 Thyroperoxidase (TPO) Antibodies, and Thyroglobulin (Tg) Antibodies.
Thyroglobulin antigen (TgAg) and TgAg washes from lymph nodes are sent out to reference labs. Cytopath slides are also processed for adequacy and reviewed with thyroid cytopathologist.
Malignant nodule missed by non-thyroidologist performing US thyroid:

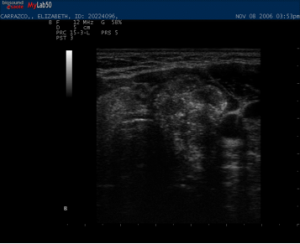
Real Time endocrine neck ultrasound with power Doppler:
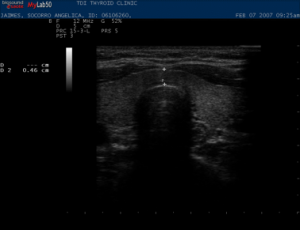
Diagnostic Ultrasound:
Ultrasound utilizes harmless sound waves to produce images of the thyroid. Ultrasound exams are done in “real-time” by Dr. Hands during an office visit. The procedure is simple and painless. The patient lies flat with the neck slightly extended, transducer gel is placed on the neck and the ultrasound probe is moved over the gland and surrounding lymph nodes. By having an expert in thyroid ultrasound perform your thyroid images you will receive immediate results, a plan on how to treat your thyroid condition and biopsy at the same time if necessary.
Pre-operative Lymph node mapping
Post-operative Thyroid cancer follow-up lymph node mapping
Parathyroid adenomas
B. Ultrasound Guided Ultrasound FNA:
FNA: (fine needle aspiration)
To better assess a thyroid nodule, a biopsy is often necessary. A fine needle aspiration biopsy (FNA) uses a small needle (smaller than most blood draw needles) to obtain cell samples from the thyroid nodule. The standard of care (best practice) is to perform this function under ultrasound guidance (using the ultrasound to determine exactly where needle is going), not free hand as is done by physicians not trained in ultrasound. This ensures that the needle tip is within the targeted nodule at the time of aspiration. Dr. Hands has preformed thousands of these procedures with insufficient results in less then 1% of samples.
Local anesthesia is not necessary, as the discomfort is similar to a blood draw. The risks are minimal, including minor bruising or discomfort and does not require any special preparation (no fasting). Patients usually return home or to work after the biopsy.
1. Cysts
2. Cancer: suspicious lymph nodes with cancer marker washings for:
a. Thyroglobulin
b. Calcitonin
c. RPMI Flow cytometry for lymphoma
3. Suspect parathyroid adenoma with PTH washings
C. Ultrasound Guided Therapeutic Interventions:
1. Percutaneous Ethanol Injections PEI for thyroid and parathyroid cysts
2. PEI for thyroid cancer lymph node ablation
Percutaneous Ethanol Injection:
This painless injection of alcohol into thyroid cysts has been a successful alternative to prevent recurrence of thyroid cysts and an alternative to surgery for recurrent cysts.
Alcohol injections have also been used as an alternative to surgery for recurrent cancer established in Lymph Nodes in the Neck. The method is effective in killing nodes with cancer and preventing continued growth. Cancer marker TG, drops after the injection and is used in patients where surgery is too risky or neck re-operation is not desired.
Dr. Hands uses ultrasound guided ethanol injections (PEI), to treat thyroid nodules that are cystic, eliminating the need for surgery. PEI can also be used to eliminate malignant lymph nodes in patients when surgery is undesired.
10. lymph node mapping pre-operatively for your surgeon,
Unfortunately, many patients in the U.S. undergo thyroid cancer surgery without Preoperative Ultrasound Mapping and, in about 15% of cases, this results in leaving behind lymph nodes (LN) to which the cancer has already spread. These cancers are then “discovered” years later during cancer follow-up exams and usually require additional surgery.
Pre-operative lymph node mapping will identify lymph nodes that can be biopsied to confirm metastasis which will extend the surgery to include removal of involved lymph nodes and increase chance of cure and decrease your chance of recurrence. The goal is to make the initial surgery the only surgery patients will need. Having to go back into a previously surgerized neck (for persistent disease, LN left behind) increases the risks of recurrent laryngeal nerve damage and hypoparathyroidism.
Pre-operative Ultrasound Mapping is performed for all patients undergoing surgery for suspected thyroid cancer. This method improves the care of the thyroid cancer patient through a team approach between the thyroid specialist and the surgeon to give you the best possible outcome. A map is drawn for the surgeon to guide the extent of surgery. With a Thyroid Center adjacent to the hospital, the surgeons can be present while Ultrasound is performed to visualize the abnormalities and plan the surgical approach. This gives the surgeon the exact location of metastatic nodes to facilitate a more comprehensive surgery. Removing involved nodes then facilitates I-131 treatment since macroscopic diseased nodes are resistant to treatment with I-131.
Post operative surveillance of your neck is performed six months after surgery, helps determine persistence or even cure of cancer.